Behaviour Change Models and Strategies
Last Updated : 01 July 2014Behaviour, the product of individual or collective action, is a key determinant of people’s health. Lifestyle risk factors are now recognised as leading contributors to morbidity and mortality in Europe. The most prevalent chronic health conditions in Europe, including cancer, cardiovascular diseases, obstructive lung diseases and diabetes, are strongly linked with lifestyle.1 Smoking, lack of physical exercise, high calorie intake and excessive alcohol consumption leading to obesity, high cholesterol levels and high blood pressure are precursors of these diseases.1 There is convincing evidence that a healthy lifestyle including regular exercise, a balanced diet, blood pressure control and smoking abstinence is associated with a longer and healthier life span.1
However, the behaviours that can cause these diseases are common and changing them may mean changing long standing habits. Many people are involved in supporting and encouraging changes in the behaviour of others and of course many seek to change their own behaviours and may seek the support of others in doing so. It is thus important to identify effective approaches and strategies that motivate change and sustain newly-adopted healthy behaviours.2
This review presents approaches to behaviour change and highlights evidence of their effectiveness. It refers to the development of theories about the processes that shape behaviour, to empirical studies that test these theories, and to applied research. The latter particularly relates to how behaviour can be changed in everyday settings and situations.
1. An ecological approach to behaviour change
There is a wide range of personal, social, and environmental factors that influence behaviour. Most can be assigned to three levels:3
- Personal or individual: beliefs, knowledge, attitudes, skills, genetics
- Social: interaction with other people including friends, family and the community
- Environmental: the area in which an individual lives, e.g. school, work place, local shops and facilities, and wider factors including the economy (such as prices) and technology.
A complex web of societal and biological factors must be considered when one aims to tackle obesity-related behaviour.4 Behaviour change is generally best served by a mix of interventions, delivered over a long period of time and modified in response to measured impact. Interventions that only address factors at the individual level, and do not take into account the social and environmental influences mentioned above, are unlikely to work. An ecological approach “that identifies and addresses the factors influencing behaviour at all three levels is likely to be most effective at bringing about behaviour change”.3 This approach also appears to be the most cost-effective.5
2. Information and advice are not enough
The traditional approach, still sometimes used in health consultations and media campaigns, relies on providing direct advice and information. While information is important for education and informing consumers, it is rarely sufficient to change behaviour. It is based on the assumptions that people lack knowledge (of what they should be doing) and that improving knowledge changes attitude, creating the desire to change.6 It does not take account of the many complex influences on behaviour. This approach prescribes changes for the client in a style that may be perceived as being “told what to do”. The health practitioner may place emphasis on the benefits of change, without fully addressing the personal implications for the individual, which may result in resistance to change.7 The same is true of many education programmes and campaigns aimed at raising awareness. The provision of information is likely to appeal to those who want to know how to change their behaviour. In turn, information provision approach may worsen health inequalities, disadvantaging those whose behaviour is more immediately shaped by their environment, and who may have less access to, or desire for, information.8
Theories and models of behaviour change
In recent years there is much interest in theories of behaviour and models of behaviour change largely drawn from psychology and informed by economics and sociology.9 They consider the wide range of psychological, social, societal and contextual factors such as emotions, habits and routines.10 The theories of change support interventions by describing how behaviours develop and change over time. Behavioural models are designed to help us understand behaviour and identify the underlying factors that influence it. An understanding of both aspects is needed to develop effective intervention strategies.11
Over 60 socio-psychological models and theories of behaviour have been identified, many of which have been used as the basis for designing and implementing health promotion programmes, with varying success.11 There is substantial evidence that the use of theory in designing and implementing behaviour change interventions improves the effectiveness of interventions.2,12 In the published studies, however, the details of the applied theory are often missing. As reviewed recently, only 44% of 34 randomised control trials in adults with obesity reported the theoretical basis of behavioural interventions.13 The most commonly applied were the Transtheoretical Model and Social Cognitive Theory (explained below), although a third of the reviewed studies did not explain why a particular theory was used. The Theory of Planned Behaviour has also been effectively applied to physical activity and dietary interventions.14,15
- Transtheoretical Model (also referred to as the ‘Stages of Change’ model): segments the audience and tailors the intervention to their stage of change: precontemplation, contemplation, preparation, action, maintenance, and termination.
- Social Cognitive Theory: focuses on the role of observing and learning from others, and on positive and negative reinforcement of behaviour.
- Theory of Planned Behaviour: assumes that people’s behaviour is determined by intention, and is predicted by attitudes, subjective norm (beliefs about whether other people approve or disapprove), and perceived behavioural control (beliefs about whether it is easy or difficult to do).
Models and theories identify techniques to change behaviour. Interventions often use several different behaviour change techniques.16 They range from providing information (for example, about the consequences of behaviour) to prompting the setting of specific goals and providing opportunities for social comparison. They can also include stress management, motivational interviewing and time management.17
3. Which behaviour change techniques are most effective?
It is not completely clear which techniques are effective under which conditions. Self-monitoring and other self-regulatory techniques (goal-setting, prompting, self-monitoring, providing feedback on performance, goal review) are consistently reported as effective behaviour change tools.18-20 A medium-to-low quality evidence suggests that dietary change is best supported by:
- instruction provision (teaching the behaviour),
- self-monitoring (recording behaviour, e.g. writing a food diary), and
- relapse prevention (problem solving and identifying coping strategies),
while physical activity is best supported by:
- prompting (to stimulate behaviour, e.g. telephone reminder),
- self-monitoring (recording behaviour, e.g. writing an activity diary),
- personalised messages (tailored to stage of change, resources and context),
- goal-setting (e.g. step-goals monitored with pedometer).18
Dietary and physical activity interventions appear to be more effective in weight management when targeted simultaneously.18 There is also good evidence to encourage engagement of social support (usually from family members).18
It is challenging to maintain behaviour change in the long-term. Evidence suggests that time management techniques (e.g., how to fit activity into a daily or weekly schedule) can help maintain physical activity levels. Encouraging self-talk (i.e. talk to yourself before and during planned behaviours) is another useful technique in facilitating physical activity and healthy eating.18
Self-determination theory
Combining skill development with underlying, intrinsic motivation and reason, is believed essential for lasting change. Intrinsic motivation does not rely on external pressure, like rewards/approval or punishment/disapproval from peers or health professionals. It exists within the individual, and is driven by interest or enjoyment in the task itself. This is the basis of the self-determination theory. Contrary to rewards and incentives, self-driven motivation is believed to be stable and enduring.21,22 The individual must believe the behaviour is enjoyable or compatible with their ‘sense of self’, values and life goals. This is supported by probing why one should persist, or in what ways the new behaviour would relate to wider goals.22 People need to feel a sense of choice and responsibility for their actions, to feel capable of achieving the goal and also understood, cared for, and valued by others.
The self-determination theory was the basis of a one-year weight-control programme involving nearly 250 individuals who had obesity or overweight. The programme used self-regulatory techniques and education about energy balance and body image. Participants were given options to reduce energy intake and to increase energy expenditure. They were encouraged to try different activities to find those they enjoy. By the end of the trial, autonomous motivation for physical activity was higher in the intervention group. In turn, physical activity levels increased by year-two and weight control at year-three. Furthermore, at year-three, women who had received the intervention reported almost 90 minutes more of moderate-to-vigorous physical activity per week than the control group. The intervention was also reported to have positively influenced eating behaviours.23
There are many parallels between the self-determination theory and motivational interviewing.23
Motivational interviewing
Motivational interviewing is a counselling approach which uses a combination of behaviour change techniques, and has been shown to be significantly more effective than traditional advice-giving. It is a directive, client-centred method for enhancing intrinsic motivation by exploring and resolving ambivalence and barriers to behaviour change.24 This approach views lecturing or confrontation as unhelpful. The main principles underpinning motivational interviewing are:8
- Express empathy (through reflective listening)
- Develop discrepancy (between the individual’s goals and their current behaviour) Avoid argumentation
- Roll with resistance (acknowledge and explore the individual’s resistance to change, rather than opposing it)
- Support self-efficacy
To gain a better understanding of the factors which impact its success, further research combining motivational interviewing with the self-determination theory has been recommended.25
Motivational interviewing is particularly effective in combination with Cognitive Behavioural Therapy (CBT).25 CBT is a treatment for emotional and behavioural problems that aims to help individuals identify and modify dysfunctional thoughts, assumptions and patterns of behaviour. It explores the range of factors that influence one’s behaviour, both external (e.g. environmental stimuli and reinforcement) and internal (e.g. thoughts). CBT also uses several techniques such as goal-setting and self-monitoring, and is based on the belief that all behaviour is learned and can be unlearned. The systematic literature review by Spahn et al. suggests that the use of an intensive course of CBT (for 6 to 12 months) may help to prevent and delay the onset of type 2 diabetes and hypertension. The potential of this intervention has also been demonstrated in treatment of childhood and adolescent obesity (30% reduction in overweight vs. 9% reduction without CBT).26
It is worth noting that these counselling approaches rely on the individual to engage in self-regulation.22,25
4. The role of social marketing
Social marketing draws on some of the principles of commercial marketing and uses behaviour change theory to influence behaviour for ‘social good’.27 The benefit is for society, not for the organisation doing the marketing. Segmentation of the relevant market allows for interventions to be targeted.
A major example of a social marketing campaign is Change4life, launched in the UK in 2009.28 It involved the government, media, industry and retailers to create a societal movement to promote healthier behaviours, making new behaviours appear fun and achievable. Ongoing support was provided to families via post and online social media (e.g. Facebook). In addition, 200,000 at-risk families received support packs, and 44,833 of these families were still interacting six months later. Over one million mothers who joined the campaign said they had made changes to their children’s behaviour.29 Another evaluation (cluster-randomised control trial) of the Change4Life campaign, revealed that while the campaign materials increased awareness of the campaign, they had little impact on the attitudes or behaviour of the study participants.30 It concluded that, in the area of childhood obesity, campaigns should be more targeted to a smaller range of behaviours and groups of people, use behaviour change theory, and use formal pilot testing.30
Social marketing as an approach to changing behaviour has been criticised, as it is hard to promote the immediate benefits of healthy lifestyle choices. Behaviour (e.g. physical activity) is not the same as a product (like running shoes), and in social marketing a consumable item is not exchanged between a producer and consumer. Therefore social marketing interventions should not be regarded as the sole means of changing behaviour.31
5. Nudging
An approach commonly known as ‘nudging’, primarily drawn from behavioural economics, has attracted interest in recent years.32 It aims to ‘nudge’ people’s choices, not by removing the less healthy ones, but by making the healthier option easier. Making salad the default side dish, or making the stairs a more attractive choice than taking the lift are examples. An individual may also be ‘nudged’ by being made aware of social norms, by receiving feedback on their behaviour compared to other people.
The reformulation of products, when recipes are modified to improve their nutritional content, is also an example.33 This approach has been effective in reducing salt intakes. Governments may also consider fiscal policies that attempt to influence food prices ‘in ways that encourage healthy eating’. However, policies may be perceived as a ‘shove’, rather than a nudge, when people are pushed to behave in ways against their will.
Unsurprisingly, there has been a lot of debate about how ethical it is to nudge people in ways that they do not notice, and whether it is effective.34 A recent influential report in the UK concluded that nudging ideally needs to be combined with other types of intervention.35
6. Using technology to change behaviour
The age of technology widens the possibilities for changing behaviour. E-health interventions, delivered using the internet, are increasingly common. They are often cited as being cost-effective, but there is a lack of data to assess this. The most effective internet-based interventions at changing behaviour appear to be more extensively based on theory (particularly the theory of planned behaviour) and use a number of techniques. The use of additional communication methods, particularly SMS (short message service) or text messaging to send motivational messages e.g. reminders of the benefits of exercise, facilitates behaviour change.15 For example a weight loss intervention study proved more effective for people who also received 2-5 personalised SMS per day, including tips and questions on different topics (and a monthly telephone call from a trained health counsellor).36 They lost more weight (1.97 kg) than the group who only received printed materials about weight control.
Mobile phones are good candidates for the delivery of behavioural interventions. The advancement of mobile technology to include internal sensors of user location, movement, emotion, and social engagement, raises the prospect of continuous and automated tracking of health-related behaviours. This supports self-regulatory techniques (e.g. goal-setting and monitoring). Such interventions may be cheaper, more convenient, or less stigmatising (due to private participation). Also, connectivity allows the sharing of behavioural and health data among health professionals or peers, which may facilitate behaviour change. There is rapid development and interest in Smartphone Apps, however research on their evaluation is still immature. The challenge will be maintaining long term use and effective behaviour change.37
Video games are another platform that engages the audience. This entertaining and interactive technology has demonstrated the ability to positively influence health-related behaviour.38 For example, a small study found that combining stationary cycling with interactive video games increased attendance and improvements in health-related physical fitness, compared to traditional cycle exercise training.39 Another study showed increased attendance with listening to music, a less expensive option.40 Controlled studies (in the laboratory) show that ‘active video games’ (which encourage physical interactivity by using body movements) result in light-to-moderate intensity physical activity, but few show significant increases.41 Video games are also an attractive platform for changing dietary behaviours, particularly to children. Research is in the early stages of understanding how such games are designed for maximum effects.42
An innovative approach for one-to-one consultations is telephone-counselling, which can provide access to remote clients. In Canada there are dedicated tele-health dietitian services, with limited evaluations (Dial-A-Dietitian, EatRight Ontario). Early evaluations suggest that this approach holds promise though more evidence is needed before standards of practice and guidelines can be developed.43
Researchers are starting to explore how online technologies can be designed to make them maximally effective.44 Given the high reach and low cost they have promise in enabling wide access.45
7. Behavioural theory in practice
Numerous frameworks aim to encourage and support the integration of behaviour change theory into the design of interventions. An example of such a framework is shown in the box below.
|
The cyclical ‘Nine Principles framework’:10 |
|
| The process is iterative; learning from one principle could require revisiting an earlier assumption. |
The differential effects on different population groups should be considered in the design and monitoring of interventions and requires a thorough understanding of the behaviour and the audience. Interventions should be targeted, based on relevant audience characteristics. Engaging the audience, so that they are partners in the process of change, seems effective at bringing about lasting change. ‘Learning through doing’ is considered to play a fundamental part in the process of change.10,11
It should be remembered that models tend to focus on personal and social factors influencing change. Additional work may be needed to identify influencing factors at the environmental level.3
The process of designing a behaviour change intervention first involves understanding the target behaviour and selecting a broad approach, and then designing the specific behaviour change techniques to be used.16 The ‘behaviour change wheel’ (Figure 1) has been developed as a guide for selecting appropriate interventions and an 'intervention design tool' is currently under development.16
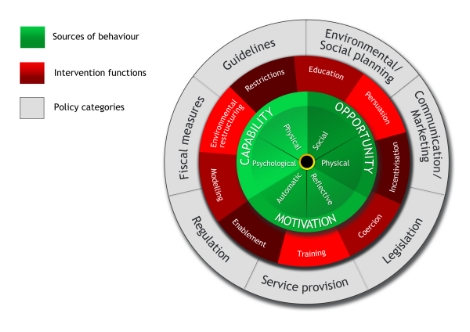
Figure 1. ‘Behaviour change wheel’
Finally, some scholars suggest focusing on social practices (patterns of action which bring together different ways of 'doing and saying').46 For example snacking may be related to the social practice of eating while watching TV. Looking at practices moves the focus away from an individual’s attitudes, behaviour and choices, and highlights how particular ways of life are sustained, including the role of governments and institutions. For example, this type of analysis would draw attention to ‘obesogenic environments’ and would consider the way in which patterns of diet and exercise are ‘socially, institutionally and infrastructurally configured’.46
8. Evaluating behaviour change interventions
Despite the recognised importance of behaviour change and the extensive research surrounding this subject, there is no consensus on how certain behaviours are best supported. Models and theories need to be used and reported in more coordinated ways to facilitate evaluation.35 To make further progress in understanding the effectiveness of behaviour change interventions, the WHO has called for all initiatives to be fully evaluated.47
Ideally, theory and evaluation will be built in from the outset of planning an intervention. Behaviour change takes time, and evaluation needs to be sufficiently long-term to demonstrate that an intervention has resulted in and maintained behaviour change. This requires the allocation of adequate funding.35 Controlled trials or other high quality methodologies should be used wherever possible. The randomised controlled trial is considered the gold standard for such evaluations, but is not always possible. Another approach is a ‘natural experiment’, where the investigator does not control who receives a treatment, but uses natural variation in exposure to the event, intervention or policy (e.g. change in nutritional requirements of school meals).35 Furthermore, evaluations will ideally have measures of behaviour as the outcome - not just measures of whether participants liked the intervention, and not just measures of the health changes (that are intended to be a consequence of targeted behaviour).12 It is critical that these measures are consistent between studies, and the details of an intervention are reported precisely.
Evaluations will help to establish whether the interventions are working and, ideally, why they are working. They will also inform decisions as to how the intervention can be improved. They should also assess the cost effectiveness of the intervention and thus discern whether or not they represent value for money.35 It is important for evidence of effectiveness to be shared between researchers, policy makers and practitioners, to avoid duplication of research and reduce costs.
9. Conclusion
Knowledge of what is successful in the field of health behaviour change is crucial for achieving improvements in health and preventing disease. In recent years, there has been growing recognition of this and a lot of work has been undertaken to examine the best approach. There is considerable evidence that the use of theory in designing and implementing health promotion programmes improves their effectiveness. However, there is less evidence concerning which techniques to use. In addition to targeting behaviours directly, interventions must help create communities and environments that enable change. Full evaluation of such interventions is essential to advance understanding of health behaviour change.
Training and continuing professional development (CPD) should reflect the shift in focus, away from simple advice-giving, towards the complexity of behaviour and the relationship between health professional and client. Developing the self-confidence of professionals to use behaviour change techniques is essential. Health professionals are advised to seek out formal training opportunities to study the principles of effective behaviour change and practise the core techniques.
References
- World Health Organization (WHO) (2008). Behaviour change strategies and health: the role of health systems. EUR/RC58/10. Tbilisi, Georgia: WHO.
- National Institute for Health and Clinical Excellence (NICE) (2007). NICE Public Health Guidance 6 ‘Behaviour change at population, community and individual levels’. London: NICE.
- Central Office of Information (COI) (2009). Communications and behaviour change. London: COI.
- Butland B, et al. (2007). Tackling obesities: future choices – project report, 2nd Edition. London: Foresight Programme of the Government Office for Science.
- Sassi F, et al. (2009). Improving lifestyles, tackling obesity: the health and economic impact of prevention strategies, in OECD Health Working Papers. Paris: OECD Publishing.
- Speller V (2007). The prevention paradox. Principles and practice of health promotion: health promotion models and theories, in HealthKnowledge Public Health Textbook, Public Health Action Support Team (PHAST).
- Britt E, et al. (2004). Motivational interviewing in health settings: a review. Patient Education and Counseling 53:147–155.
- Christmas S (2009). Nine big questions about behaviour change. London: Department for Transport.
- Michie S, et al. (2008). From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Applied Psychology: an international review 57(4):660–680.
- Darnton A (2008). Practical Guide: An overview of behaviour change models and their uses. London: Government Social Research Service (GSR).
- Darnton A (2008). Reference report: an overview of behaviour change models and their uses. London: GSR.
- Michie S & Johnston M (2012). Theories and techniques of behaviour change: Developing a cumulative science of behaviour change. Health Psychology Review 6(1):1-6.
- Dombrowski, et al. (2007). Current issues and future directions in Psychology and Health: Towards a cumulative science of behaviour change: Do current conduct and reporting of behavioural interventions fall short of best practice? Psychology & Health 22(8):869-874.
- McEachan RRC, et al. (2011). Prospective prediction of health-related behaviours with the theory of planned behaviour: A meta-analysis. Health Psychology Review 5(2):97-144.
- Webb TL, et al. (2010). Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research 12(1):e4.
- Michie S, van Stralen NM & West R (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science 6:42.
- Abraham C & Michie S (2008). A taxonomy of behavior change techniques used in interventions. Health Psychology 27(3):379–387.
- Greaves CJ, et al. (2011). Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 11:119.
- World Cancer Research Fund (WCRF) (2009). Effective health behaviour change strategies. Informed 35.
- Michie S, et al. (2009). Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychology 28(6):690-701.
- Teixeira PJ, et al. (2012). Motivation, self-determination, and long-term weight control IJBNPA 9:22
- Teixeira PJ, et al. (2011). Why we eat what we eat: the role of autonomous motivation in eating behaviour regulation. Nutrition Bulletin 36(1):102-107.
- Silva MN, et al. (2008) A randomized controlled trial to evaluate self-determination theory for exercise adherence and weight control: rationale and intervention description. BMC Public Health 8:234.
- Rubak S, et al. (2005). Motivational interviewing: a systematic review and meta-analysis. British Journal of General Practice 55(513):305-312.
- Spahn JM, et al. (2010). State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. Journal of the American Dietetic Association 110(6):879-891.
- Teixeira PJ, et al. (2012). The role of self-determination theory and motivational interviewing in behavioral nutrition, physical activity, and health: an introduction to the IJBANPA special series. IJNBPA 9:17.
- Stead M, Hastings G & McDermott L (2007). The meaning, effectiveness and future of social marketing. Obesity Reviews 8(s1):189-193.
- UK Department of Health (2011). Changing behaviours, improving outcomes: a new social marketing strategy for public health. London: Department of Health.
- UK Department of Health (2010). Change4Life one year on. London: COI for the Department of Health and the Department for Children, Schools and Families.
- Crocker H, Lucas R & Wardle J (2012). Cluster-randomised trial to evaluate the ‘Change for Life’ mass media/ social marketing campaign in the UK. BMC Public Health 12:404.
- Rayner M (2007). Social marketing: how might this contribute to tackling obesity? Obesity Reviews 8(s1):195-199.
- Thaler RH & Sunstein CR (2008). Nudge: improving decisions about health, wealth, and happiness. New Haven, CT & London: Yale University Press.
- EU project EATWELL (Interventions to Promote Healthy Eating Habits: Evaluation and Recommendations) (2012). Effectiveness of Policy Interventions to Promote Healthy Eating and Recommendations for Future Action: Evidence from the EATWELL Project.
- Blumenthal-Barby JS & Burroughs H (2012). Seeking better health care outcomes: the ethics of using the “nudge". American Journal of Bioethics 12(2):1-10.
- House of Lords (2012). Behaviour change. Science and Technology Select Committee 2nd Report of Session 2010–12. London : The Stationery Office Limited.
- Patrick K, et al. (2009). A text message–based intervention for weight loss: Randomized Controlled Trial. Journal of Medical Internet Research 11(1):e1.
- Dennison L, et al. (2013). Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. Journal of Medical Internet Research 15(4):e86.
- Baranowski T, et al. (2008). Playing for real: video games and stories for health-related behavior change. American Journal of Preventative Medicine 34(1):74-82.
- Warburton DE, et al. (2007). The health benefits of interactive video game exercise. Applied Physiology, Nutrition, and Metabolism 32(4):655-663.
- Adamo KB, Rutherford JA & Goldfield GS (2010). Effects of interactive video game cycling on overweight and obese adolescent health. Applied Physiology, Nutrition, and Metabolism 35(6):805-815.
- Peng W, Crouse JC & Lin JH (2013). Using active video games for physical activity promotion: a systematic review of the current state of research. Health Education & Behavior 40(2):171-192
- Baranowski T, Diep C, Baranowski J (2013). Influences on children's dietary behavior, and innovative attempts to change it. Annals of Nutrition & Metabolism 62(Suppl 3):38-46.
- Myers EF, et al. (2010). Nutrition and telephone counseling: future implications for dietitians and teledietetics. Topics in Clinical Nutrition 25(2):88-108.
- Morrison LG, et al. (2012). What design features are used in effective e-health interventions? A review using techniques from critical interpretive synthesis. Telemedicine journal and e-Health 18(2):137-144.
- Cugelman B, et al. (2011). Online interventions for social marketing health behavior change campaigns: a meta-analysis of psychological architectures and adherence factors. Journal of Medical Internet Research 13(1):e17.
- Shove E (2010). Beyond the ABC: climate change policy and theories of social change. Environment And Planning 42(6):1273-1285.
- World Health Organization (WHO) (2008). Resolution. Behaviour change strategies and health: the role of health systems. EUR/RC58/R8. Regional Committee for Europe Fifty-eighth session. Tbilisi, Georgia: WHO.



