Antimicrobial resistance (Q&A)
Last Updated : 21 November 2023Antibiotic resistance represents one of the most significant global threats to health and food security in the world today. Overuse and misuse of these life-saving drugs have allowed bacteria to evolve defences against them at an alarming rate. If left unaddressed, antibiotic resistance could lead to a future where common human infections and minor injuries may once again be harder to treat. In this article, we will explore the topic of antibiotic resistance, seeking to understand how and why it occurs, how it impacts humanity, and what measures can slow its rise.
What is antimicrobial resistance (AMR), and how is it different from antibiotic resistance?
An antimicrobial is a general term used for any drug (e.g., antibiotics, antivirals, antifungals and antiparasitics) that works to treat and prevent infections caused by microorganisms, such as viruses, bacteria, fungi and parasites, by killing or inhibiting their growth. Antimicrobial resistance (AMR) happens when a microorganism becomes resistant to an antimicrobial drug that used to be effective in treating the infections it causes.
Antibiotic resistance, on the other hand, is a sub-category of antimicrobial resistance. It refers specifically to the resistance of bacteria to antibiotic drugs, the drugs used specifically to treat infections caused by bacteria, such as urinary tract infections or pneumonia.1
When was antibiotic resistance first discovered, and when did it become a serious threat?
Alexander Fleming discovered penicillin (the first antibiotic used for treating bacterial infections) in 1928. He already warned about the potential for bacteria to evolve resistance as early as 1945.2 As he and other researchers predicted, once mass production of antibiotics took place in the 1950s and 1960s, resistance began to emerge in hospitals and communities. Through the 1980s and 1990s, many common bacteria continued to develop resistance to older drugs due to the overuse of antibiotics in health care and agricultural production, and the World Health Organization and the European Centre for Disease Prevention and Control documented alarming increases in resistant pathogens across Europe and globally.3
Statistics from the European Union/European Economic Area (EU/EEA) currently estimate that over 670,000 infections and 33,000 deaths are a direct consequence of infections caused by antibiotic-resistant bacteria each year. This means that when individuals become ill with infections caused by these resistant bacteria, the standard antibiotics are no longer effective in treating them. As a result, the treatment options become limited, leading to prolonged illness, increased healthcare costs, and in some cases, death.4
Why does antibiotic resistance occur?
Antibiotic resistance occurs naturally over time as bacteria gradually evolve to become resistant to the drugs aimed at destroying them. When antibiotics are used to treat a bacterial infection, some bacteria can already have an inherent resistance mechanism, which helps them survive the treatment. Those bacteria survive and pass on the resistance as they multiply, creating a new bacterial population more resistant to the antibiotic. That antibiotic therefore becomes less effective in treating infections caused by those specific bacteria. In some situations, the resistant gene can also be transferred to other types of bacteria, further spreading the resistance to that drug.5
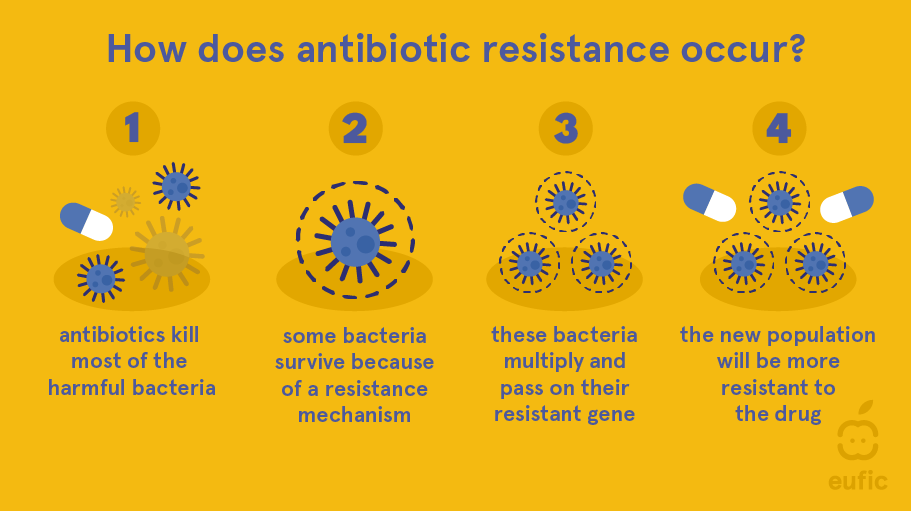
The evolution of resistance in bacteria is a natural occurrence, but human activity is accelerating the process. Resistance will not develop each time an antibiotic is used, but the more an antibiotic is used, the more chances there are for resistance to develop. When antibiotics are misprescribed for viral infections or used too broadly in animal production (as part of animal feed), it fuels the development and spread of resistant bacteria. In short, while resistance is a natural response to any antibiotic use over time, the misuse and overuse of antibiotics speed up the process.4
Once resistant, how do bacteria spread resistance?
Resistant bacteria can also spread their resistance genes to other bacteria, even different species. This happens primarily through the so-called “horizontal gene transfer,” a process that allows bacteria to acquire new traits from unrelated types of bacteria living nearby by swapping resistance genes. For example, viruses that infect bacteria can accidentally carry genes from one infected bacterial cell to another. Bacteria can also connect to exchange genes directly or absorb DNA from dead or broken bacteria around them. This sharing of genes allows bacteria to rapidly acquire traits like antibiotic resistance from neighbours, even if they didn't initially have that ability themselves.
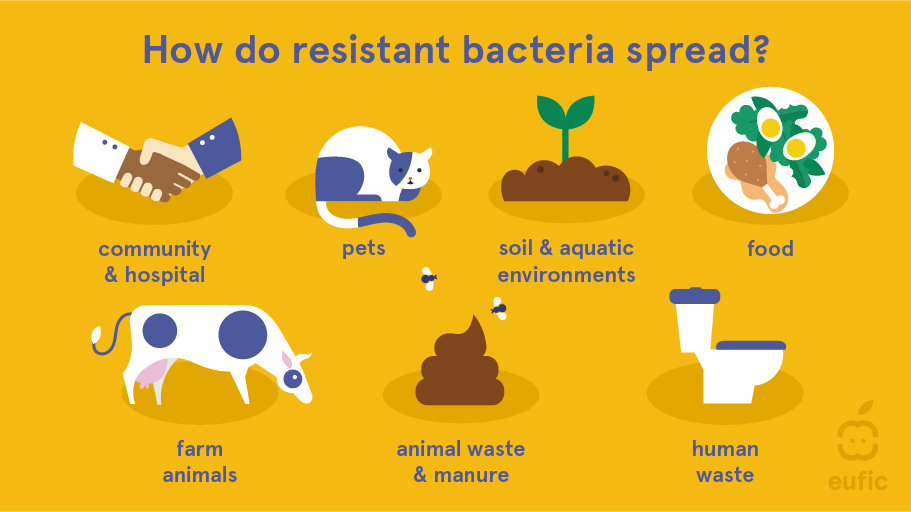
While overprescription and misuse of antibiotics exacerbate the development and spread of resistance, poor hygiene in healthcare facilities, farms and slaughterhouses is also an important contributor to its spread. Resistant bacteria in waste (from humans and pets in sewage) and farm animals (from use in manure as fertiliser) can contaminate the environment and get into the water supply, which is then used to irrigate crops and as drinking water. Traces of the resistant bacteria can remain on those crops and in the water and then be ingested by humans and animals. Meat from farm animals can also be contaminated with resistant bacteria, which humans can ingest if the meat is undercooked or food hygiene practices are not followed (e.g., cross-contamination in the kitchen).2,3,5
Why is growing resistance so worrying?
Our healthcare system relies on reliable access to effective antibiotics. Antimicrobial resistance not only jeopardises modern medicine's ability to perform high-risk procedures safely, but it can also turn once easily treatable infections into life-threatening conditions if antibiotics fail. If drug resistance continues to spread, it could trigger a situation where common illnesses and minor, easily fixable injuries may once more become life-threatening or fatal.1
Is antibiotic resistance permanent or reversible?
Antibiotic resistance in bacteria is generally considered permanent since once the resistance genes are acquired, they are typically not lost. However, bacteria may lose resistance genes if they are no longer exposed to antibiotics. This can happen over many generations as the bacteria adapt to their environment without antibiotics, where non-resistant bacteria outcompete the resistant ones.
It is important to note that even if resistance is lost in a population of bacteria, the resistance genes are still present in the environment and can be transferred to other bacteria through various mechanisms like horizontal gene transfer. Thus, resistance can re-emerge if antibiotics are reintroduced to the environment.
Therefore, while antibiotic resistance may not always be permanent at the individual bacterial level, it is a persistent problem requiring continuous management and intervention. Preventing the spread of resistance and judicious use of antibiotics are key strategies for minimising the impact of this global health challenge.2
What actions can slow resistance development?
Improved antibiotic stewardship, banning non-therapeutic use in agriculture, developing alternative disease prevention methods like vaccines, rapid diagnostics to fine-tune prescribing, and public education on hygiene and medicine disposal all offer hope to extend antibiotic effectiveness for the coming decades as new drugs are brought to market more slowly. International cooperation will also be vital in combating the issue.6
How can I help reduce the spread of antibiotic resistance?
To help reduce the spread of antibiotic resistance, there are several actions you can take:
- Only use antibiotics when prescribed by a certified health professional: antibiotics should be used only when necessary and appropriate. Follow your healthcare provider's instructions and avoid self-medicating with antibiotics.
- Prevent infections through good hygiene practices: regularly wash your hands with soap and water, especially before handling food and after using the bathroom. Practice safe food handling and preparation and avoid close contact with sick individuals.
- Complete the full course of antibiotics: if you are prescribed antibiotics, make sure to take the full course as prescribed, even if you start feeling better. This helps ensure that all bacteria causing the infection are eliminated.
- Do not share or use leftover antibiotics: antibiotics should not be shared with others or used for future illnesses. Unused antibiotics should be properly disposed of according to local guidelines.
- Stay up to date on vaccinations: vaccinations can help prevent infections in the first place, reducing the need for antibiotics.
By following these guidelines, you can play an important role in combating antibiotic resistance and protecting both your health and the health of future generations.7

 This article was produced in collaboration with HOLiFOOD. HOLiFOOD has received funding from the European Union’s Horizon 2020 Research and Innovation programme under Grant Agreement No. 101059813.
This article was produced in collaboration with HOLiFOOD. HOLiFOOD has received funding from the European Union’s Horizon 2020 Research and Innovation programme under Grant Agreement No. 101059813.
References
- World Health Organization: WHO. Antimicrobial resistance. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance. Published November 17, 2021.
- Rosenblatt-Farrell N. The landscape of antibiotic resistance. Environ Health Perspect. 2009;117(6):A244-A250. https://doi.org/10.1289/ehp.117-a244
- Irfan M, Almotiri A, AlZeyadi ZA. Antimicrobial Resistance and Its Drivers—A Review. Antibiotics. 2022; 11(10):1362. https://doi.org/10.3390/antibiotics11101362
- Cassini A, Högberg LD, Plachouras D, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infec
- Larsson, D.G.J., Flach, CF. Antibiotic resistance in the environment. Nat Rev Microbiol 20, 257–269 (2022). https://doi.org/10.1038/s41579-021-00649-x
- Velazquez-Meza ME, Galarde-López M, Carrillo-Quiróz B, Alpuche-Aranda CM. Antimicrobial resistance: One Health approach. Vet World. 2022;15(3):743-749. https://doi.org/10.14202/vetworld.2022.743-749
- World Health Organization: WHO. Antibiotic resistance. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance. Published July 21, 2020.