Vitamin D: foods, functions, how much do you need & more
Last Updated : 11 January 2021Vitamin D, sometimes also referred to as “the sunshine vitamin”, is an important vitamin that we can get not only from food but also from a bit of sunlight.
What is vitamin D?
Vitamin D is a fat-soluble vitamin that we can get from foods, but also produce in our bodies when the skin is directly exposed to the sun. Food sources of this vitamin are particularly important during the times when our exposure to sunlight is lower, such as during the autumn and winter months.
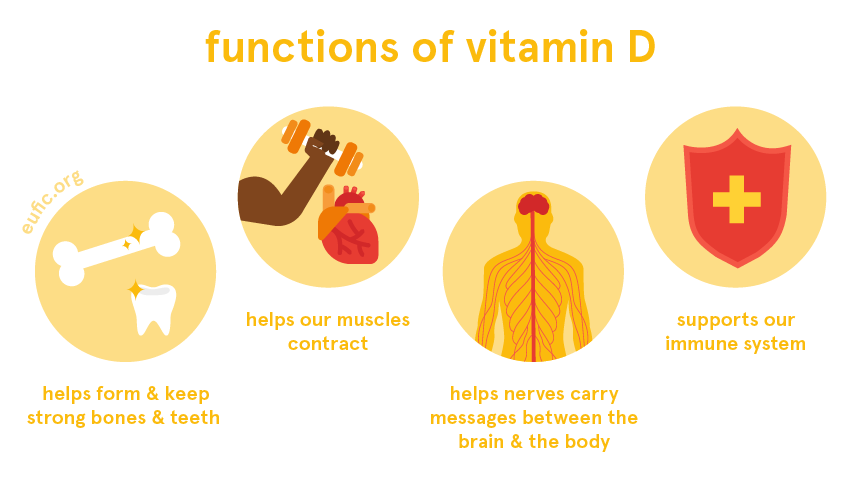
What are the functions of vitamin D?
Vitamin D acts as a hormone in our bodies, regulating many processes that keep us healthy. One of the main functions of vitamin D is to help balance the levels of calcium and phosphorus in our bodies, which are needed to form our bones and teeth, to help our muscles contract, to help nerves carry messages between the brain and the body and to keep our cells functioning well. Vitamin D is also important to support the healthy function of our immune system.
How much vitamin D do I need per day?
How much vitamin D you need per day changes according to your age, sex and life-stage.
The dietary reference value (DRV)* for healthy adults (over the age of 18), including during pregnancy and lactation, is for 15 μg of vitamin D per day.
We can get the recommended amounts of vitamin D by eating vitamin D rich foods and have regular sun exposure. However, in some cases, supplements are needed to help meet the needs for this vitamin (see below who needs to pay extra attention to their vitamin D intake). Following your country's dietary guidelines on a healthy and balanced diet will help you meet your needs for vitamin D.
If you are afraid that you’re not getting enough vitamin D, we recommend that you consult a qualified nutritionist or dietitian to discuss how to best meet your own nutritional needs.
* These values are based on the adequate intake (AI) estimates from European Food Safety Authority (EFSA). They should not be interpreted as nutrient goals. To know more about DRVs in Europe click here.
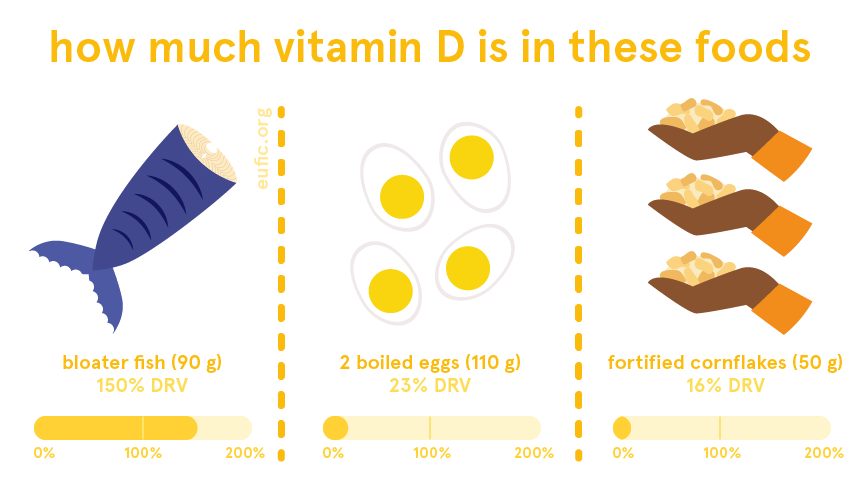
What foods contain vitamin D?
Some of the richest foods in vitamin D include:
- fatty fish (such as herring, salmon and mackerel)
- meat (particularly organ meats) and meat products
- egg yolks
- fortified foods.
Some mushrooms are also natural sources of vitamin D, but the content varies on the amount and duration of UV-B light exposure, during growth and/or production.

Does vitamin D interact with other nutrients?
Vitamin D is particularly important to help our bodies absorb calcium and phosphorus from foods as well as to help them build and keep strong bones and teeth. This process also uses vitamin K, which is why we need a good balance of all these micronutrients to keep optimal bone growth and health.
What happens if I have too little vitamin D?
We can get a deficiency in vitamin D when we don’t get enough exposure to sunlight, when we don’t have or don’t absorb enough vitamin D from foods, or when our kidneys don’t properly convert vitamin D to its active form in our bodies.
Low levels of vitamin D can impair our bodies’ ability to absorb calcium and phosphorus from foods, which then need to be moved from our bones to supply the rest of the body. Over time, this causes our bones to become less dense (with less bone mass) and weaker. In children it can lead to rickets, a condition that causes bones to become weak and soft, often affecting the normal growth of bones such as causing the bowing of the legs’ bones. In adults, it leads to osteomalacia, a similar condition in which bones become soft. It can also cause pain in muscles and an increased risk of falls or bone fracture.
In the long-term, vitamin D deficiency increases the risk of osteoporosis, particularly among the elderly or after menopause/andropause. Osteoporosis, also known as “brittle bones”, is a disease that causes bones to become very weak and fragile, increasing the risk of bone fracture.
What happens if I have too much vitamin D?
It’s virtually impossible to get too much vitamin D from sun exposure because our bodies are quite efficient at regulating this process. Most people will make enough vitamin D from being out in the sun for short periods of time (15 to 30 minutes). However, keep in mind that we should avoid unprotected sun exposure for more than 30 minutes. Remember to wear sunscreen and protective clothing and limit sun exposure in the midday sun.
Excessive intakes of vitamin D are usually caused by the overuse of vitamin D supplements, which can increase calcium levels in the blood to toxic levels. Over time, it can cause calcium to accumulate in the soft tissues (such as blood vessels, organs, etc) which can lead to heart and kidney damage.
In general, adults are advised not to have more than 100 μg of vitamin D per day, which is about six times the DRV for this vitamin.
Before taking vitamin D supplements, check with your doctor or a registered dietitian/nutritionist or consult your national dietary guidelines.
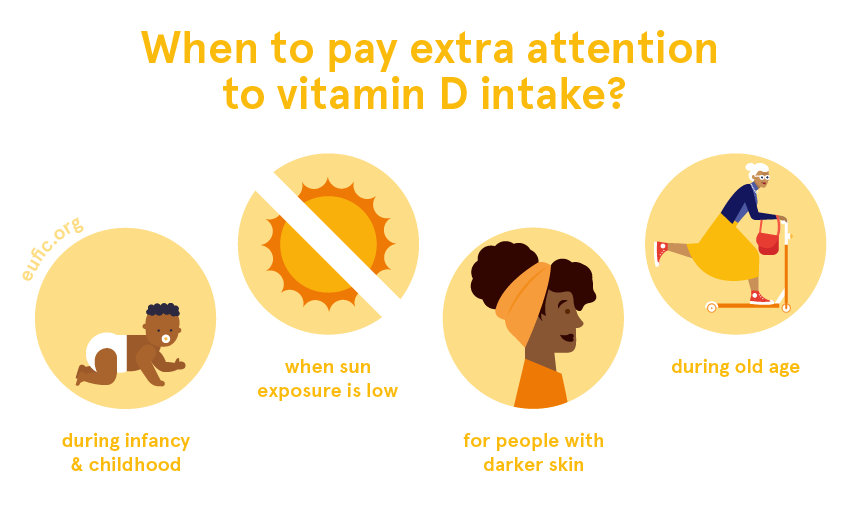
When should I pay extra attention to a vitamin D deficiency?
Our bodies make vitamin D when our skin is directly exposed to the sun, which is why people with low sun exposure are more prone to having lower levels of this vitamin. This can include people who live in countries with long periods of low sun exposure (such as the winter months in Northern Europe) or people who regularly fully cover their bodies with clothing (such as in some cultures or religions).
People with darker skin also need to keep their vitamin D levels in mind, because the skin pigment melanin reduces the production of vitamin D.
With age, our bodies have less capacity to make vitamin D and we’re also more likely to stay indoors, which reduces our sun exposure. Particularly, the elderly need to keep good intakes of vitamin D, as it helps to increase the calcium absorption from foods and to face health problems such as osteoporosis.
References
- European Food Safety Authority. 2016. Scientific opinion on dietary reference values for vitamin D. EFSA Journal 2016;14(10):4547
- World Health Organization (WHO). 2004. Vitamin and mineral requirements in human nutrition. 2nd edition. Geneva, Switzerland: WHO.
- Public Health England. 2019. McCance and Widdowson’s Composition of Foods Integrated Dataset.



