Calcium: foods, functions, how much do you need & more
Last Updated : 11 January 2021We’ve probably all heard that calcium makes our bones strong and healthy at least once in our childhood. But is that all that we need it for?
What is calcium?
Calcium is one of the major minerals, which our bodies need in relatively larger amounts to keep healthy. We can find calcium in many animal- and plant-based foods, as well as in drinking water.
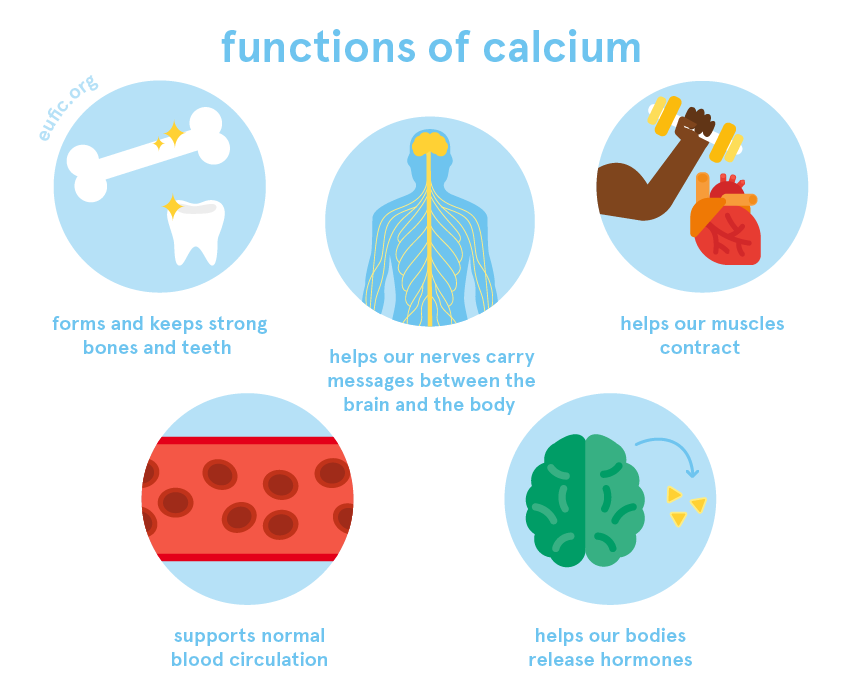
What are the functions of calcium?
One of the key roles of calcium, together with phosphorus, is to form and keep our bones and teeth strong. In fact, it’s in our bones and teeth where we find 99% of our calcium stored. The remaining is used for other vital functions such as to help our blood vessels contract and relax (thus, supporting our normal blood circulation), keeping our hearts beating, moving our muscles and helping our nerve cells carry messages (nerve impulses) between the brain and the body. Calcium is also a key element to activate different enzymes and helps our bodies release hormones.
How much calcium do I need per day?
How much calcium you need per day changes according to your age, sex and life-stage.
The dietary reference value (DRV)* for healthy adults (over the age of 18) including during pregnancy and lactation, is between 950-1000 mg of calcium per day.
We can get enough calcium from our diets by eating a variety of foods. Following your country's dietary guidelines on a healthy and balanced diet will help you meet your needs for calcium.
If you are planning to change your diet, have recently done so, or are concerned that you might not be getting enough calcium, we recommend that you consult a qualified nutritionist or dietitian to discuss how to best meet your own nutritional needs.
* These values are based on the population reference intake (PRI) estimates from the European Food Safety Authority (EFSA). They should not be interpreted as nutrient goals. To know more about the DRVs in Europe click here.
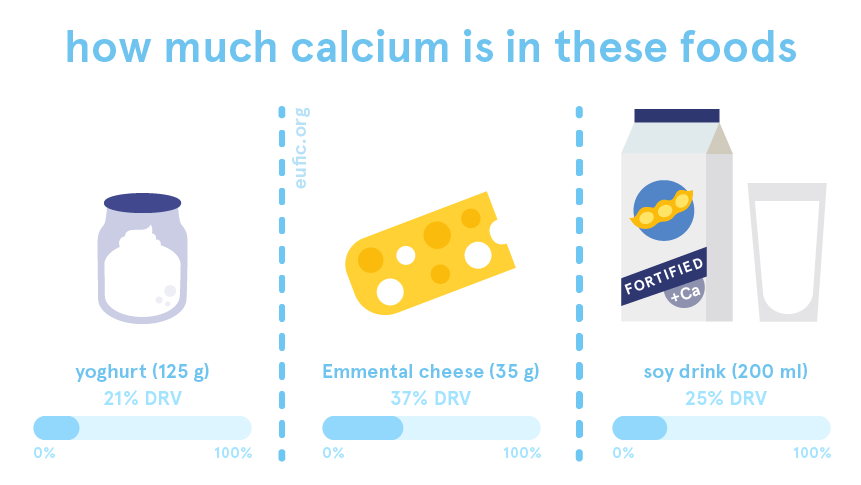
What foods contain calcium?
We can find calcium in a variety of foods, as well as in drinking water.
The amount of calcium in water is usually higher in regions where water has a high mineral content, also called hard water.
Some foods rich in calcium include:
- dairy products
- dark green vegetables (such as spinach, purslane, chard, endive and broccoli)
- legumes
- nuts
- fish with soft bones (such as canned sardines)
- fortified foods, such as plant-based alternatives to milk and yoghurt.
Many herbs and seeds are also rich sources of calcium, however, contrary to some misconceptions, they don’t really increase our calcium intake because we only eat them in very small amounts.

Does calcium interact with other nutrients?
Sodium, phosphorus and vitamin D affect the levels of calcium in our bodies in different ways, making it important to have a good balance of all these micronutrients in the diet.
For example, diets high in salt (sodium chloride) can reduce the levels of calcium in our bodies, even if we regularly include good amounts of calcium in our diets. This is because our bodies use the calcium stored in our bones to get rid of the excess of salt through urine. As so, respecting the recommended intake of salt, is important not only to lower the risk of cardiovascular diseases but also to protect the health of our bones.
Similarly, a diet high in phosphorus and low in calcium can lower the levels of calcium in our bodies by preventing its absorption in the gut. The contrary is also true, a diet high in calcium and low in phosphorus can reduce the absorption of phosphorus. Any of these two scenarios can have negative consequences on the health of our bones, making it important to have a good balance of both minerals in our diets.
Lastly, vitamin D plays a key role in keeping healthy levels of calcium in our bodies, since it helps the absorption of calcium from foods, supports the release of calcium from bones when needed and reduces the amount of calcium lost in the urine.
What happens if I have too little calcium?
Diets low in calcium are particularly harmful to the health of our bones. Bone is a living tissue that is constantly being broken down and replaced with calcium. To keep this process balanced, we need to get enough calcium from our diets to replace what’s lost throughout our life. Plus, when we don’t have enough calcium in our diets, our bodies pull calcium out of our bones to keep the levels of this mineral in our blood and muscles at a normal level. Over time, this can reduce our bone mass and cause our bones to become weak.
In children, calcium deficiency increases the risk of rickets, a disease that makes the bones softer and weak. If it sets at an early age, it causes stunted growth and the bowing of long bones.
In adults, calcium deficiency will also lead to the softening and weakening of bones, which in this case is called osteomalacia. Over a long period of time, it increases the risk of osteoporosis, a health condition when bones become very weak and break easily.
What happens if I have too much calcium?
Calcium from foods is not considered harmful since it’s very unlikely that we get too much of it through our diets alone. However, it’s possible to get high doses of this mineral from calcium supplements, particularly if taken together with vitamin D.
Healthy adults, including during pregnancy and lactation, are advised not to have more than 2500 mg of calcium per day, which is around three times the DRV for calcium.
Toxic levels of calcium in our bodies are mainly related to health conditions that cause calcium to accumulate in our blood. In the long-term, it can lead to health consequences such as muscular weakness, irregular heart beating, kidney disease and the accumulation of calcium in our soft tissues (such as organs, muscles and blood vessels) and consequent damage.
There is some evidence suggesting that high-dose calcium supplementation (not dietary calcium) – possibly over 1,000 mg/d – may increase the risk for cardiovascular diseases, although evidence is mixed.4-7 A possible explanation is that supplemental calcium leads to rapid increases in levels of circulating calcium, disturbs the calcium balance, and increases the risk of calcium deposits in our large arteries causing them to harden and stiffen which increases the risk of developing atherosclerosis. However, authoritative bodies such as the National Osteoporosis Foundation and the American Society for Preventive Cardiology both affirm that calcium from food or supplements is safe from a cardiovascular standpoint (as long as doses do not exceed the tolerable upper level of intake). They found no relationship (beneficial or harmful) with cardiovascular disease and cerebrovascular disease risk, mortality, or all-cause mortality in healthy adults.8
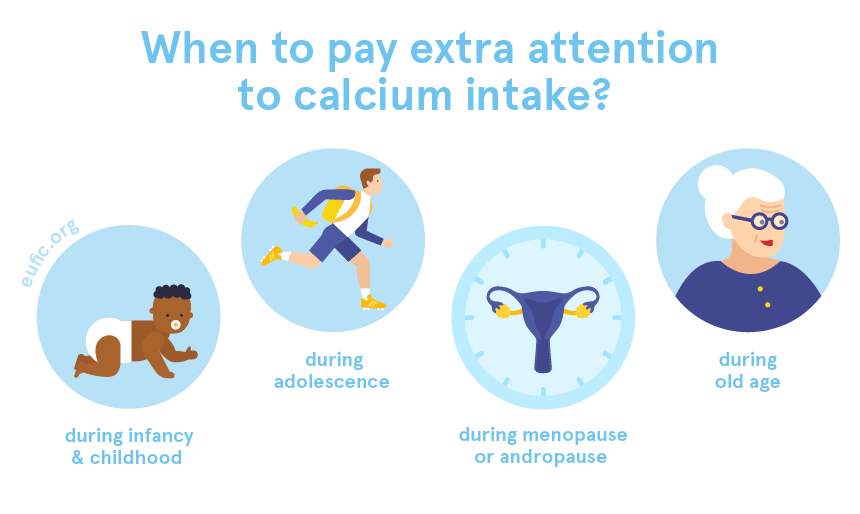
When should I pay extra attention to my calcium intake?
It’s important to have good amounts of calcium in our diets at any age, but there are some phases when low intakes can affect us more.
For example, calcium is particularly important to growing healthy and strong bones, making it a key mineral during periods of fast growth and development. Those include our infancy and childhood (0-9 years old), but also during adolescence and puberty.
On another hand, as we age our bodies tend to absorb less calcium and from the onset of menopause or andropause, we start to lose bone faster. This puts the elderly (over 65 years of age), or those at menopause/andropause, at higher risk of developing osteoporosis. Combining a healthy lifestyle with adequate sources of calcium in our diets are two key factors to protect our bone health during this phase.
References
- European Food Safety Authority. 2015. Scientific Opinion on Dietary Reference Values for calcium. EFSA Journal 2015;13(5):4101, 82
- World Health Organization (WHO). 2004. Vitamin and mineral requirements in human nutrition. 2nd edition. Geneva, Switzerland: WHO.
- Public Health England. 2019. McCance and Widdowson’s Composition of Foods Integrated Dataset.
- Yang, C., Shi, X., Xia, H., Yang, X., Liu, H., Pan, D., & Sun, G. (2020). The evidence and controversy between dietary calcium intake and calcium supplementation and the risk of cardiovascular disease: a systematic review and meta-analysis of cohort studie
- Anderson, J. J., Kruszka, B., Delaney, J. A., He, K., Burke, G. L., Alonso, A., ... & Michos, E. D. (2016). Calcium intake from diet and supplements and the risk of coronary artery calcification and its progression among older adults: 10‐year follow‐up of
- Myung, S. K., Kim, H. B., Lee, Y. J., Choi, Y. J., & Oh, S. W. (2021). Calcium supplements and risk of cardiovascular disease: A meta-analysis of clinical trials. Nutrients, 13(2), 368.
- Huo, X., Clarke, R., Halsey, J., Jackson, R., Lehman, A., Prince, R., ... & Trialists’Collaboration, C. S. T. (2023). Calcium supplements and risk of CVD: A meta-analysis of randomized trials. Current Developments in Nutrition, 7(3), 100046.
- Kopecky, S. L., Bauer, D. C., Gulati, M., Nieves, J. W., Singer, A. J., Toth, P. P., ... & Weaver, C. M. (2016). Lack of evidence linking calcium with or without vitamin D supplementation to cardiovascular disease in generally healthy adults: a clinical gu



